Scientific References
In this section of the website, internationally renowned experts share with us their scientific opinion on specific topics related to Nutrition. If you are interested in improving your knowledge and learning about the latest research on obesity, allergies and other compelling topics, this page is for you! Sponsorship Disclosure: Many of the publications, programs, conferences, educational resources and other content available on this website have been funded and/or prepared by the Nestle Nutrition Institute or its Nestle affiliates.

Effect of protein intake and weight gain velocity on body fat mass at 6 months of age: The EU Childhood Obesity Programme
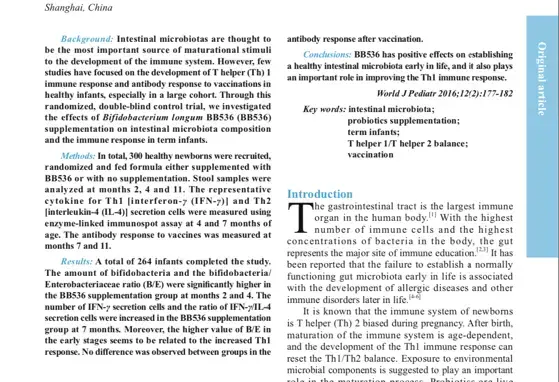
Effects of Bifidobacterium supplementation on intestinal microbiota composition and the immune response in healthy infants

Lower protein in infant formula is associated with lower weight up to age 2 y: a randomized clinical trial1–4
Occurrence of Lactobacillus reuteri in human breast milk
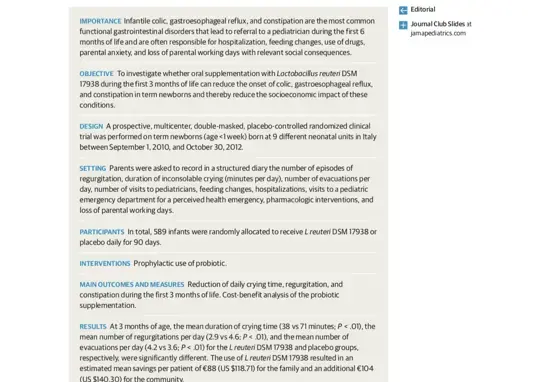
Prophylactic Use of a Probiotic in the Prevention of Colic, Regurgitation, and Functional Constipation

Efficacy of Lactobacillus GG in prevention of nosocomial diarrhea in infants
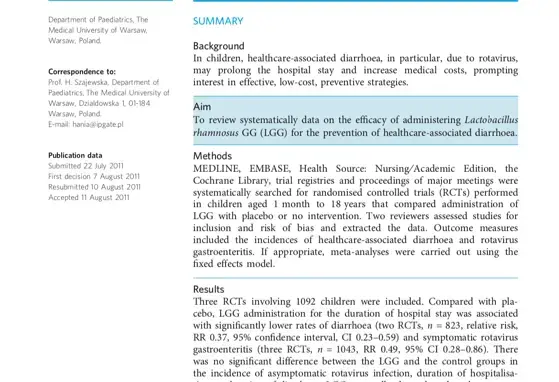
Meta-analysis: the effects of Lactobacillus rhamnosus GG supplementation for the prevention of healthcare-associated diarrhoea in children

Vertical transmission of Malaria in a public maternity of Luanda, Angola (The transmission of malaria from a pregnant woman to the fetus)

Effect of probiotic supplementation in the first 6 months of life on specific antibody responses to infant Hepatitis B vaccination