The Impact of Metabolic Syndrome in India

Obesity has been one of the fastest growing public health burdens in India for the past two decades, and there is no end in sight to the rise of type 2 diabetes and the metabolic syndrome. The scale of the problem is staggering. Currently, around one-third of the population in India are living with metabolic syndrome, the majority of them being women.1 Increasing inactivity and Westernization of the Indian diet are partly to blame. Multinational fast food companies with huge advertising budgets have radically changed the way in which Indian adults and children eat, and the rush to copy the Western model has led to even easier access to unhealthy food choices. The story is similar throughout the developing world, but the risk of obesity and metabolic syndrome has important consequences specific to the Indian people and other South Asian populations.
Not all bodies are created equal
To understand the impact of metabolic syndrome in India, we have to look at the defining characteristics of body composition among the population. Compared with white Caucasians, Asian Indians store more body fat, particularly in the abdomen and in areas where fat is less often found, such as the liver, neck and between the fibres of the muscles.2 These fat stores are essentially toxic, and increase each of the risk factors for diabetes and metabolic syndrome. But what puts the Asian Indian population at even higher risk of these diseases is that this increased fat storage occurs at a lower body mass index than among Caucasians.3 In India, even so-called ‘non-obese’ people can have severe metabolic disturbances (see figure). Around a quarter of this group have insulin resistance, a fundamental risk factor for diabetes. Research has shown that sensitivity to blood sugars among Asian Indians without heart disease is similar to that of British heart attack survivors.
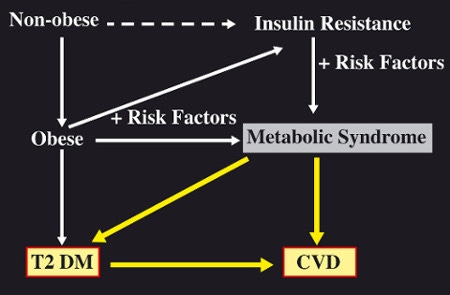
The relationship of obesity with insulin resistance, the metabolic syndrome and cardiovascular disease in India
It dosen’t stop there. We have also discovered evidence to suggest that fat that gathers just below the skin of the abdomen (‘subcutaneous fat’), rather than fat stored around the abdominal organs (‘visceral fat’), may be more damaging to metabolic health in South Asians than in other races. This is especially worrying as Asian Indians have more subcutaneous fat than Caucasians even at birth, and this is associated with higher levels of the hormones insulin (which controls the metabolism of carbohydrates and fats) and leptin (which controls appetite).
The pathway to metabolic syndrome and how to stop it in its tracks
Childhood obesity is widespread in India. As a consequence, the presence of abnormal levels of fat and cholesterol in the blood (‘dyslipidaemia’) is seen as early as 15 years of age, and increases steeply after 20. Diabetes develops an average of 10 years earlier than in Western populations, at around 30–35 years of age. With the onset of metabolic syndrome the body starts to age more quickly, impacting a person’s health and ability to work. Early death from heart disease and other complications associated with metabolic syndrome is common.
It is clear that early identification of metabolic syndrome is important. The good news is that India already has some of the world’s largest programmes for intervention in childhood obesity, focusing on lifestyle changes known to help prevent diabetes and heart disease in later life. If parents and teachers can be educated about healthy eating and physical activity, and pass on that information to children while still in school, it could solve half the problem of metabolic syndrome in India.
The other half of the problem is to educate people who are already living with, or are at high risk of, diabetes and metabolic syndrome. More money and resources should be available for early screening and detection of disturbed metabolism. Currently, doctors rarely have enough time during clinic visits to provide the advice that patients need on eating healthily, exercising regularly and quitting smoking. Poor training on prevention of disease means that an estimated 70% of the Indian population does not receive correct lifestyle advice from their doctor.
The changing face of metabolic syndrome in India
We need more research into novel ways of intervening in the diet of Asian Indians, and that much more data are needed from across the developing world. As with other countries like Brazil, the face of metabolic syndrome in India has been changing. Whereas diabetes and metabolic syndrome used to mainly affect the rich, these days it is more likely to be the rural and semi-urban poor who are affected. The Indian government has recently become aware of this change, and is now focusing their screening efforts on people living in slums and on others with low incomes.
See our other experts opinion

Low-Protein Formula Slows Weight Gain in Infants of Overweight Mothers

ACHIEVING OPTIMAL FEEDS FOR PRETERM BABIES, RECOMMENDATIONS: AND REALITIES IN PRACTICE: NIGERIAN PERSPECTIVE

Human Milk Oligosaccharides – Compositional Analysis and Metabolism in Infants