Probiotics are live, non-pathogenic microorganisms that provide benefits on human gut health. Studies have shown that probiotics colonize the gut and compete with pathogenic microorganisms, thereby suppressing the growth of harmful bacterial colonies.1 Probiotics are increasingly being administered in the healthcare setting, particularly in the pediatric population, despite the prevailing uncertainty on their efficacy and their appropriate clinical use. To address this need, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Working Group (WG) on Probiotics published an updated set of practical recommendations that specify the indications for the use of probiotics for selected pediatric gastrointestinal disorders. 2
Summary of Recommendations
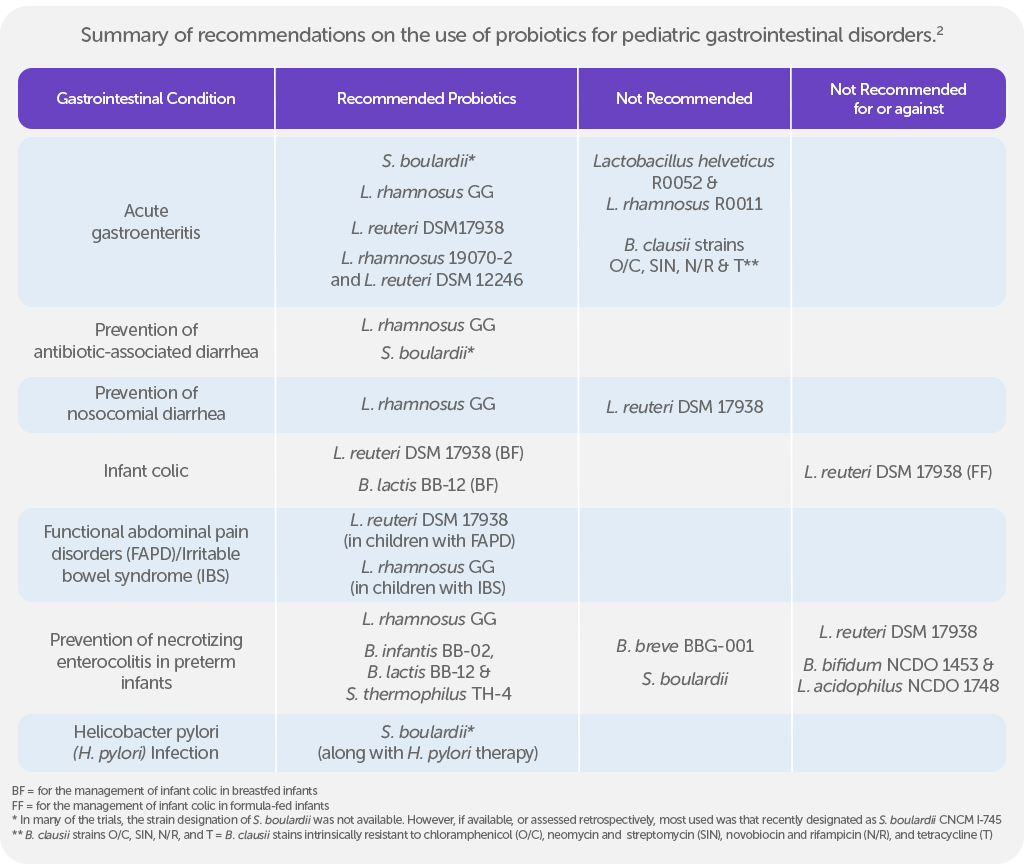
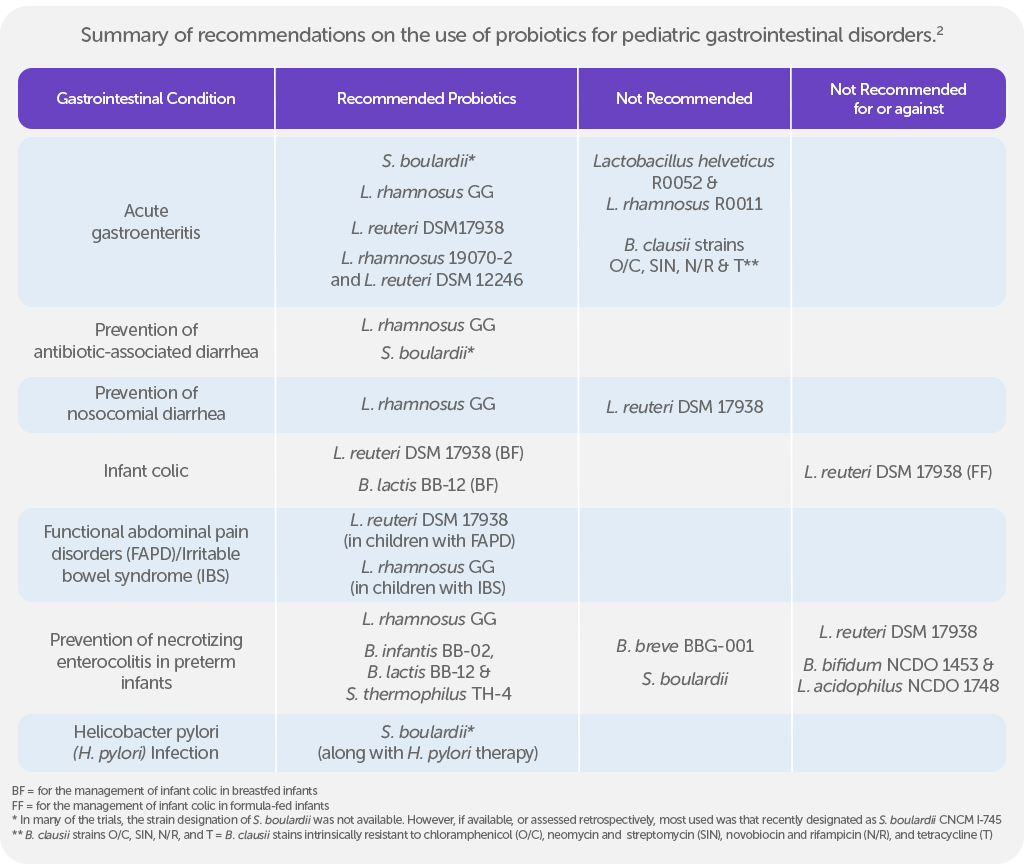
The ESPGHAN WG formulated the updated recommendations for appropriate clinical use of probiotics based on systematic reviews and/or meta-analyses and randomized controlled trials (RCTs) that were published until 2021. The included studies compared probiotic use (in any form and dose) with no probiotics (placebo or no treatment). Studies on probiotic-supplemented formulas were excluded.2
The review considered recent evaluations by ESPGHAN and previous guidelines, focusing on probiotics as defined by international standards. The WG did not provide general recommendations but focused on specific probiotic strains or combinations, requiring at least two RCTs per strain for recommendations.2
ESPGHAN recommends Saccharomyces (S) boulardii or Lacticaseibacillus rhamnosus (L. rhamnosus) GG to prevent antibiotic-associated diarrhea (AAD). Probiotic administration should start as early as possible, simultaneously to the antibiotic treatment and continue throughout the duration of the therapy.2
For managing acute gastroenteritis, apart from rehydration and suitable feeding, the WG recommends considering administration of S. boulardii, L. rhamnosus GG, Limosilactobacillus reuteri (L. reuteri) DSM 17938, or the combination of L. rhamnosus 19070-2 and L. reuteri DSM 12246 for 5 days in most cases as these may reduce the duration of diarrhea.2
The group also recommends the use of L. reuteri DSM 17938 and Bifidobacterium lactis (B. lactis) BB-12 in managing infant colic in breastfed infants, for a minimum of 21 days, as they have been shown to decrease crying time.2
To help prevent necrotizing enterocolitis (NEC) in preterm infants, ESPGHAN recommends L. rhamnosus GG or a combination of three probiotic strains including Bifidobacterium (B) infantis BB-02, B. lactis BB-12, and Streptococcus thermophilus (S. thermophilus) TH-4.2
Notably, the ESPGHAN WG has no recommendations for or against the use of probiotics in ulcerative colitis, celiac disease and small intestinal bacterial overgrowth. No probiotic strains were found to be effective in managing functional constipation, and there is no available data on probiotic use in pancreatitis.
The recommendations are intended to be broadly applied and viewed as the preferred approach to management.2
Further studies that elucidate the efficacy, as well as the specific strain, dose, and duration of probiotic administration in the healthcare setting are still required to establish unifying clinical guidelines on the use of probiotics for the pediatric population.
References:
- Bodke H and Jogdand S. Role of Probiotics in Human Health. Cureus. 2022 14(11):e31313. doi: 10.7759/cereus.31313.
- Szajewska H, et al; ESPGHAN Special Interest Group on Gut Microbiota and Modifications. Probiotics for the Management of Pediatric Gastrointestinal Disorders: Position Paper of the ESPGHAN Special Interest Group on Gut Microbiota and Modifications. J Pediatr Gastroenterol Nutr. 2023 Feb 1;76(2):232-247. doi: 10.1097/MPG.0000000000003633.